
This patient population is known to suffer from a 14-fold increased risk of dying from sudden cardiac death (SCD) compared to patients with cardiovascular diseases without known renal impairment. Interesting examples in this context are studies in haemodialysis (HD) patients. Apart from an emergency setting, (clinical) studies could also benefit from a non-invasive, rapid, and cost-efficient tool for diagnosis of electrolyte imbalance. Incidence and determinants of hyperkalemia and hypokalemia in a large healthcare system,” Int. This could allow for early diagnosis and improvement of strategies to optimize treatment and consequently improve patient outcomes in emergency settings. and for all use cases, a rapid non-invasive point-of-care (POC) diagnostic tool is desirable. Similar to potassium, the impairment of other electrolyte concentrations is also highly relevant in clinical practice, 1 1. Ong, “Ĭompetency-based critical care,” in Renal Failure and Replacement Therapies, edited by S. Impairment of potassium homeostasis is common and can be iatrogenic, for example, caused by the use of diuretic drugs or due to diseases, e.g., chronic kidney disease (CKD), myocardial infarction, etc. Furthermore, we demonstrate the potential of computational modeling approaches to gain insight into the mechanisms of relevant clinical findings and as a tool to obtain synthetic data for methodical improvements in monitoring approaches. Differences in the findings from automatic monitoring studies are discussed, and current studies utilizing machine learning are presented demonstrating the potential of the deep learning approach. Selected clinical studies are presented, supporting or questioning the use of the ECG for the monitoring of electrolyte concentration imbalances. In this review, we present the current state of potassium and calcium concentration monitoring using the ECG and summarize results from previous work. The electrocardiogram (ECG) could meet this need and becomes an established diagnostic tool allowing home monitoring of the electrolyte concentration also by wearable devices.
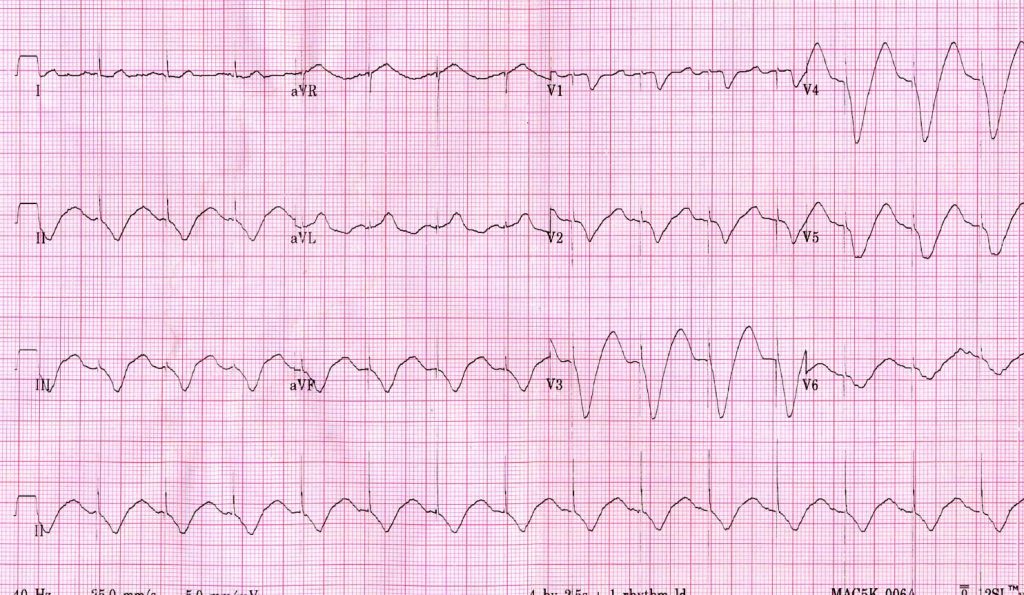
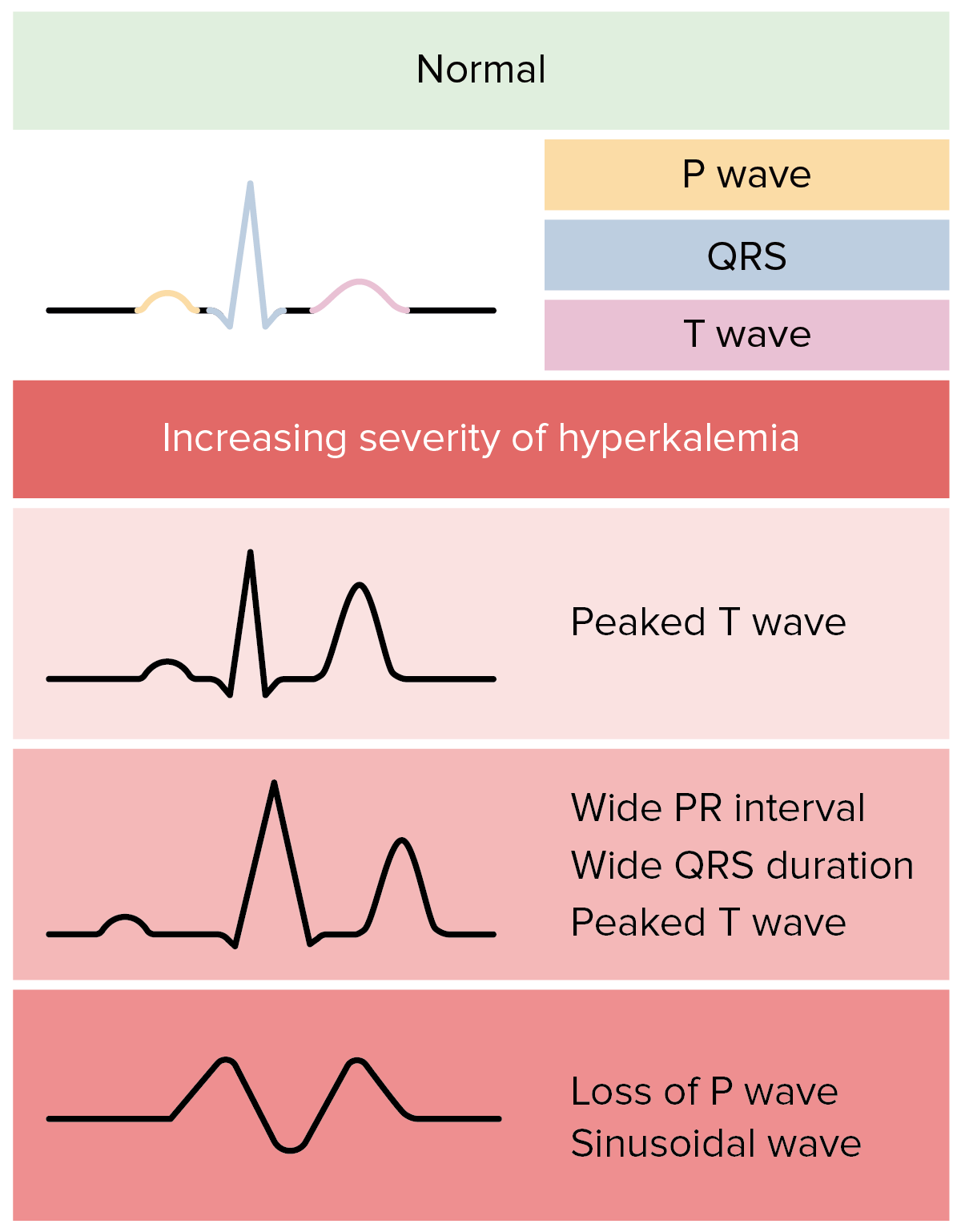
A rapid and non-invasive point-of-care method is yet needed. The clinically established method for the diagnosis of electrolyte concentration imbalance is blood tests. 3 Finally, excessive body potassium can be removed with sodium polystyrene sulfonate (Kayexalate), whereas hemodialysis represents the definitive method to reduce serum potassium levels.Diseases caused by alterations of ionic concentrations are frequently observed challenges and play an important role in clinical practice. 2 Sodium bicarbonate, beta-2 adrenergic agonists, and the combination of glucose and insulin all drive potassium intracellularly and lower the extracellular serum potassium level. 3 Calcium (intravenous calcium chloride or gluconate) can effectively block the effect of extracellular potassium elevation on cardiac myocytes within minutes by restoring a more appropriate electrical gradient across the cellular membrane. 1 – 3 Treatment of life-threatening hyperkalemia focuses on blocking the effects on myocyte transmembrane potential and cardiac conduction, as well as decreasing extracellular potassium levels. Typical ECG findings in hyperkalemia progress from tall, “peaked” T waves and a shortened QT interval to lengthening PR interval and loss of P waves, and then to widening of the QRS complex culminating in a “sine wave” morphology and death if not treated. Diagnosis of hyperkalemia is usually based on laboratory studies, although the electrocardiogram (ECG) may contain changes suggestive of hyperkalemia.


 0 kommentar(er)
0 kommentar(er)
